The Invisible Weight of Worry
Sarah stared at her laptop screen, the deadline for her project looming just hours away. Instead of working, she found herself caught in a familiar spiral of thoughts: "What if I miss something important? Why can't I just focus? Everyone else seems to handle this so easily." Her ADHD had made starting the project difficult, but now that she was finally seated at her desk, it was anxiety keeping her paralyzed. The tasks that seemed manageable yesterday now felt overwhelming, creating a perfect storm of worry and inaction.
This pattern of overthinking, rumination, and anxiety isn't just Sarah's personal struggle—it's a common experience for many adults with ADHD. The relationship between ADHD and anxiety is complex, intertwined, and often misunderstood, leaving many feeling trapped in a cycle of worry.
struggle—it's a common experience for many adults with ADHD
Breaking It Down: What's This All About?
ADHD and anxiety are two distinct conditions that frequently travel together, creating a challenging neurological partnership. ADHD (Attention-Deficit/Hyperactivity Disorder) is primarily characterized by difficulties with attention, hyperactivity, and impulsivity, while anxiety involves excessive worry and fear responses. What makes this combination particularly challenging is how these conditions feed into each other, creating a self-reinforcing cycle.
When these conditions co-occur, the experience goes beyond simple distraction or occasional nervousness. It creates a unique neurobiological state where executive function struggles combine with heightened emotional responses, making everyday tasks feel significantly more difficult to manage.
Why This Matters
Understanding the relationship between ADHD and anxiety matters because this combination affects approximately 50% of adults with ADHD, making it one of the most common comorbidities. This dual challenge impacts daily functioning, emotional well-being, and overall quality of life in profound ways that go beyond either condition alone.
For those experiencing this combination, the impact can be seen in:
Significantly greater difficulty initiating and completing tasks
Heightened emotional reactivity to stress
Increased likelihood of perfectionism and self-criticism
The development of "analysis paralysis" where decision-making becomes overwhelming
Reduced work performance and greater interpersonal challenges
Higher rates of sleep disturbances and physical health issues
The good news is that recognizing this connection is the first step toward effective management strategies that address both conditions simultaneously.
Myths vs. Facts: Setting the Record Straight
❌ Myth 1: ADHD and anxiety are completely separate issues that should be treated independently
→ ✅ Fact: Research shows ADHD and anxiety share overlapping neurobiological pathways and often require integrated treatment approaches that address both conditions.
❌ Myth 2: Anxiety in people with ADHD is just a psychological reaction to living with ADHD
→ ✅ Fact: While ADHD challenges can certainly trigger anxiety, there are shared neurobiological mechanisms involving the prefrontal cortex, amygdala, and neurotransmitter systems that create a genuine neurological connection between these conditions.
❌ Myth 3: Stimulant medications for ADHD always make anxiety worse
→ ✅ Fact: Although stimulants can sometimes increase anxiety in some individuals, research shows they can actually reduce anxiety in many people with ADHD by improving executive function and reducing the stress of managing ADHD symptoms.
❌ Myth 4: Rumination and overthinking in ADHD are the same as in other anxiety disorders
→ ✅ Fact: ADHD-related rumination tends to be more task-related, future-oriented, and self-critical, often revolving around executive function challenges rather than the more general worry patterns seen in primary anxiety disorders.
❌ Myth 5: People with ADHD who experience "analysis paralysis" just need to try harder to take action
→ ✅ Fact: Analysis paralysis in ADHD represents a genuine neurological state where executive function deficits combine with anxiety responses, creating a physiological barrier to action that goes beyond simple procrastination or laziness.
The Science Behind It
The fascinating connection between ADHD and anxiety begins in the brain, where several key regions and systems play crucial roles in both conditions.
Neuroanatomical Connections
Research using advanced brain imaging has revealed significant overlaps in the brain regions affected by both ADHD and anxiety:
The prefrontal cortex (PFC), critical for attention, organization, executive function, and emotional regulation, often shows reduced volume and delayed maturation in ADHD. This same region is crucial for cognitive flexibility and decision-making processes that are impaired in anxiety.
The amygdala, central to processing emotions (especially fear), shows altered connectivity with the prefrontal cortex in individuals with ADHD. Studies have found smaller amygdala volume associated with both ADHD risk and symptom severity, while amygdala hyperactivation occurs during emotional processing tasks.
The anterior cingulate cortex (ACC) plays a vital role in attentional processing, emotional regulation, and conflict monitoring. Research has shown reduced activation of the dorsal ACC in ADHD patients when responding to fear cues, while increased functional connectivity between the amygdala and rostral ACC has been linked to higher emotional lability.
The default mode network (DMN) and task-positive network (TPN) balance is particularly relevant. In individuals with ADHD, the DMN (active during rest or daydreaming) often remains engaged even when focused attention is required, contributing to mind-wandering and ruminating thoughts. This persistent DMN activity has been linked to difficulties in stopping rumination.
Neurotransmitter Systems
The chemical messengers in the brain also reveal important connections between ADHD and anxiety:
Dopamine, crucial for motivation, reward, attention, and emotional regulation, shows reduced levels or impaired signaling in ADHD. This dysregulation not only affects core ADHD symptoms but may also contribute to rumination through its role in the brain's reward system and motivation.
Norepinephrine, essential for attention, alertness, and stress response, is often deficient in ADHD—the first disorder to be associated with norepinephrine imbalance. Given its role in stress response, norepinephrine dysregulation can contribute to heightened anxiety and worry.
Serotonin deficiency is closely associated with both depression and anxiety disorders, and imbalances can exacerbate ADHD symptoms like emotional dysregulation and impulsivity. Evidence suggests serotonin imbalances may play a role in negative thinking and rumination in individuals with ADHD.
GABA (Gamma-Aminobutyric Acid), the primary inhibitory neurotransmitter, promotes calm and reduces anxiety. Studies have found reduced GABA concentration in children with ADHD, potentially contributing to both ADHD symptoms and anxiety through decreased inhibitory control.
ADHD symptoms like emotional dysregulation and impulsivity.
The Executive Function Connection
Executive functions—the higher-level cognitive skills that help us organize, plan, and regulate behavior—provide another critical link:
Core executive function deficits in working memory, inhibition, and emotional self-regulation make it difficult to mentally organize and manage thoughts, potentially leading to rumination.
Difficulties with planning, task initiation, and time perception can create a build-up of uncompleted responsibilities, triggering worry about potential negative consequences.
Research has demonstrated a positive correlation between executive function deficits and higher levels of both worry and rumination, with rumination being more strongly associated with executive dysfunction.
Treatment Recommendation Insights:
For mild to moderate combined symptoms: Starting with CBT combined with mindfulness practices often provides a solid foundation.
For more severe ADHD symptoms with secondary anxiety: Carefully monitored medication (starting with either stimulants or non-stimulants based on anxiety severity) combined with therapy typically works best.
For severe anxiety with ADHD: Non-stimulant medications or carefully titrated stimulants plus CBT focused on anxiety management often yields best results.
For significant emotional dysregulation: DBT skills training can be particularly beneficial when added to other treatment approaches.
Making It Work: How to Apply This in Real Life
✅ Step 1: Break the Rumination Cycle – Recognize when you're caught in overthinking.
✨ Positive Point: Using the "thought labeling" technique (simply noting "That's ruminating thinking") creates distance from the thought cycle.
⚠️ Negative Point: Without awareness, rumination can continue for hours, consuming mental energy that could be directed toward action.
✅ Step 2: Implement the Two-Minute Rule – If a task takes less than two minutes, do it immediately.
✨ Positive Point: Creates momentum and prevents small tasks from becoming anxiety-triggering backlogs.
⚠️ Negative Point: Even two-minute tasks can trigger overthinking if you don't have a clear system for implementing this rule.
✅ Step 3: Create External Structure – Use visual reminders and organizational systems.
✨ Positive Point: Reduces cognitive load and executive function demands that can trigger anxiety.
⚠️ Negative Point: Too many systems or overly complicated structures can become overwhelming and counterproductive.
✅ Step 4: Practice Strategic Procrastination – Schedule worry time.
✨ Positive Point: Containing worry to specific times prevents it from constantly interrupting productivity.
⚠️ Negative Point: Requires consistent practice and might initially feel unnatural or ineffective.
✅ Step 5: Develop an Action Hierarchy – Create a simple 1-3 rating for tasks.
✨ Positive Point: Simplifies decision-making and prevents analysis paralysis.
⚠️ Negative Point: May still require effort to implement when anxiety is high.
✅ Step 6: Build a Mindfulness Practice – Start with 5 minutes daily.
✨ Positive Point: Strengthens the neural pathways that counter rumination and improves present-moment awareness.
⚠️ Negative Point: Benefits accumulate gradually over time rather than providing immediate relief.
✅ Step 7: Implement Body-Based Interventions – Use physical activity strategically.
✨ Positive Point: Even brief movement can shift brain state away from rumination and anxiety.
⚠️ Negative Point: Can be difficult to initiate when caught in analysis paralysis.
Real-Life Examples in Action
Michael's Story: "I'd always been a chronic overthinker, spending hours ruminating about work tasks without actually starting them.
After my ADHD diagnosis at 36, I realized this wasn't just anxiety—it was the intersection of my ADHD and anxiety. My psychologist taught me to recognize when my default mode network was 'stuck on' and to use physical movement as a pattern interrupt.
Now when I notice myself overthinking, I immediately stand up, do 10 jumping jacks, and then focus on taking just the first small step of the task. This simple routine has cut my rumination time down by about 70% and significantly increased my productivity."
Elena's Experience: "The worst part of my ADHD-anxiety combination was always the 'analysis paralysis' around decisions.
I would research options endlessly, afraid of making the wrong choice. My therapist helped me create a decision-making framework with time limits for different types of decisions. Small decisions get 5 minutes max, medium ones get 30 minutes of research, and only genuinely important decisions get more extensive consideration.
I also learned to recognize that my ADHD brain was seeking the dopamine hit from research rather than the anxiety-producing decision itself. Setting these boundaries has freed up so much mental energy that I was previously wasting on trivial choices."
Jamie's Transformation: "Managing my medication was a game-changer. I had been told that stimulants would make my anxiety worse, so I avoided them for years despite struggling terribly with focus.
When I finally worked with a psychiatrist who specialized in ADHD-anxiety comorbidity, she explained that my anxiety was largely secondary to my ADHD challenges.
We carefully started a low dose of stimulant medication while monitoring my anxiety levels. Surprisingly, as my ADHD symptoms improved, most of my anxiety diminished too. I still use CBT techniques for the remaining anxiety, but the combination approach targeting both conditions has been transformative for my quality of life."
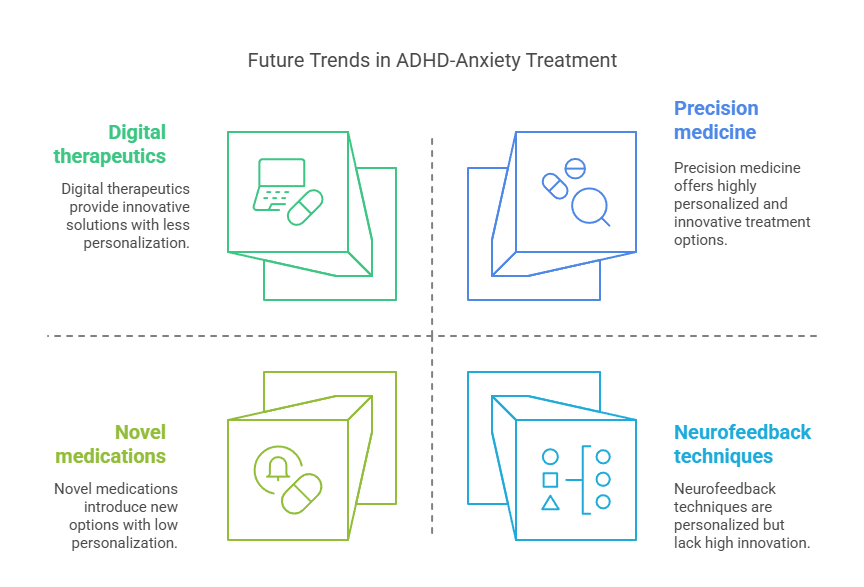
Future Trends: What's Next in ADHD-Anxiety Treatment
The landscape of ADHD and anxiety treatment is evolving rapidly, with several promising developments on the horizon:
🔮 Precision medicine approaches are gaining momentum, with emerging research focused on identifying biomarkers that can predict which treatments will work best for specific individuals with ADHD-anxiety comorbidity.
This could potentially reduce the trial-and-error approach currently necessary in medication selection.
📈 Digital therapeutics are showing promise in recent clinical trials, with FDA-approved applications specifically designed to address cognitive challenges at the intersection of ADHD and anxiety.
These technologies offer accessible, on-demand support that complements traditional treatments.
👥 Neurofeedback techniques are advancing beyond experimental stages, with newer protocols specifically targeting the default mode network dysregulation common in combined ADHD and anxiety.
Early research shows promising results for reducing rumination and improving cognitive flexibility.
🧠 Novel medications targeting glutamate systems are in development, potentially offering new options for those who don't respond well to current pharmacological approaches.
These might address both ADHD and anxiety symptoms through different mechanisms than existing medications.
⚡ Transcranial magnetic stimulation (TMS) protocols specifically designed for ADHD-anxiety comorbidity are showing promising results in preliminary studies, potentially offering a non-pharmaceutical option for treatment-resistant cases.
These emerging approaches suggest a future where treatment can be increasingly personalized to the specific neurobiological profile of each individual's ADHD-anxiety presentation.
Frequently Asked Questions
❓ Question 1: Can ADHD cause anxiety, or are they just frequently co-occurring conditions?
💡 Answer: Both are true. While ADHD and anxiety can exist as separate conditions, research confirms that ADHD itself can directly contribute to anxiety through several
mechanisms: the chronic stress of managing executive function challenges, neurobiological overlap in affected brain regions, and shared neurotransmitter imbalances. Studies show that approximately 50% of adults with ADHD also experience anxiety disorders—a rate significantly higher than in the general population.
❓ Question 2: How can I tell if my rumination is ADHD-related or primarily anxiety-driven?
💡 Answer: ADHD-related rumination tends to have specific characteristics: it's often focused on uncompleted tasks, perceived failures in executive function, or future-oriented worries about performance. It frequently involves self-criticism about productivity or organization. In contrast, primary anxiety rumination is typically more generalized, may involve more catastrophic thinking about safety or health, and is less tied to specific executive function challenges. Understanding this distinction can help guide treatment approaches.
❓ Question 3: Will treating my ADHD automatically improve my anxiety?
💡 Answer: Not necessarily, though it often helps significantly. Research shows that effective ADHD treatment improves anxiety in 50-60% of cases where the anxiety is secondary to ADHD challenges. However, if you have a primary anxiety disorder alongside ADHD, you'll likely need treatment approaches specifically targeting both conditions. A comprehensive assessment can help determine the relationship between your ADHD and anxiety symptoms and guide appropriate treatment planning.
❓ Question 4: Can mindfulness really help with ADHD when focusing is already difficult?
💡 Answer: Yes, though it requires adaptation. Traditional mindfulness practices can indeed be challenging for people with ADHD, but modified approaches show significant benefits. Research demonstrates that shorter, more frequent mindfulness sessions (even 3-5 minutes) can be effective, especially when combined with movement or using external anchors for attention. Regular practice gradually strengthens attention networks while reducing default mode network activity associated with rumination.
Cultural & Geographical Variations
The experience and treatment of ADHD-anxiety comorbidity shows interesting variations across different cultures and regions:
🌍 Diagnostic approaches vary significantly across countries. Northern European countries like Finland and Sweden tend to view ADHD from a more neurobiological perspective and commonly address the anxiety component as part of comprehensive ADHD treatment. In contrast, some Mediterranean and Asian countries more often diagnose and treat anxiety first, sometimes overlooking underlying ADHD.
📊 Medication preferences show strong regional patterns. The US typically favors pharmacological approaches for both conditions, with approximately 62% of adults with ADHD-anxiety comorbidity receiving medication. European countries generally use medications more selectively, with greater emphasis on psychosocial interventions, particularly in countries like Germany and France.
🔍 Traditional practices in East Asian countries frequently incorporate mindfulness and body-based interventions alongside conventional treatments. Japanese approaches often integrate attention-training practices derived from traditional meditation with modern ADHD treatments, showing promising outcomes for managing the rumination component of ADHD-anxiety.
Learning from these diverse approaches suggests that integrative models combining pharmacological, psychological, and cultural practices may offer the most comprehensive support for individuals with this complex comorbidity.
Pro Tips & Insider Insights
🧠 Befriend your brain's DMN-TPN balance: Understanding when your default mode network (mind-wandering mode) is overactive can help you intentionally engage your task-positive network through brief, focused activities that require full attention.
⏱️ Implement the "10-10-10 Rule" for breaking anxiety-paralysis: Work for just 10 minutes, take a 10-minute break, and repeat 10 times. This structure bypasses the overwhelming feeling of starting while creating sufficient momentum.
🌊 Use "worry surfing" rather than fighting anxious thoughts: When rumination hits, imagine your thoughts as waves—observe them rise and fall without getting caught in their undertow. This mindfulness technique reduces the grip of rumination without requiring you to stop the thoughts forcefully.
🧪 Track your stimulant medication's impact on anxiety with a simple 1-10 scale: Rate your anxiety before taking medication and at 1-2 hour intervals afterward. This data helps identify whether your medication is helping or exacerbating anxiety symptoms.
📱 Set up anxiety "speed bumps" on your devices: Use app timers and website blockers that create a 10-second pause before accessing anxiety-triggering content (like email or social media). This brief delay is often enough to interrupt automatic rumination patterns.
Potential Challenges & Solutions
🚧 Challenge 1: Medication that helps ADHD symptoms increases anxiety
🛠️ Solution: Work with your healthcare provider to explore modified dosing (sometimes lower doses or divided doses throughout the day can reduce anxiety while still helping ADHD). Consider adding alpha-2 agonists like guanfacine or clonidine, which can address both ADHD symptoms and anxiety. Time-release formulations often provide smoother effects with less anxiety than immediate-release options.
🚧 Challenge 2: Implementing organizational systems feels overwhelming
🛠️ Solution: Start with a single, simple system focused on capturing tasks rather than organizing them. The "capture first, organize later" approach reduces executive function load. Consider a "brain dump" notebook where you write everything down without categorizing, then spend 10 minutes at the end of each day transferring only the most important items to your actual organizational system.
🚧 Challenge 3: Mindfulness practice is difficult to maintain
🛠️ Solution: Instead of scheduled meditation sessions, implement "mindful transitions" between activities—30-second moments of presence when moving between tasks. Attach mindfulness to existing habits (like waiting for coffee to brew or brushing teeth) rather than creating a new habit. Use guided mindfulness specifically designed for ADHD from resources like the TARA method or Mindfulness for ADHD programs.
🚧 Challenge 4: Rumination intensifies at night, disrupting sleep
🛠️ Solution: Create a "worry download" routine 1-2 hours before bed. Write all concerns on paper using two columns: "Things I can take action on tomorrow" and "Things outside my control." For actionable items, schedule specific times to address them the next day. For items outside your control, practice acceptance statements. Use a body-based relaxation technique like progressive muscle relaxation rather than thought-based techniques before sleep.
Measuring Success: Specific Metrics & Milestones
Quantitative Metrics:
📏 Rumination Duration: Measure the average time spent in rumination cycles daily. Baseline: Track for one week to establish your starting point. Target: Reduce by 25% after one month, 40% after three months.
📏 Task Initiation Rate: Track the percentage of planned tasks successfully started without delay. Baseline: Typically 30-40% for those with ADHD-anxiety. Target: Increase to 60% within two months, 75% within six months.
📏 Sleep Onset Latency: Measure time from going to bed to falling asleep. Baseline: Over 45 minutes for many with evening rumination. Target: Reduce to under 30 minutes within one month, under 20 minutes within three months.
📏 Worry Episode Frequency: Count distinct worry episodes daily. Baseline: Establish personal baseline for one week. Target: Reduce frequency by 30% within six weeks.
Milestone Achievements:
🏆 Rumination Recognition: Consistently noticing rumination within 2-3 minutes of onset (vs. being caught in it for extended periods).
🏆 Decisive Action: Successfully making decisions within appropriate timeframes based on decision importance without excessive information-seeking.
🏆 Emotional Recovery: Reducing recovery time from anxiety spikes by 50% using learned techniques.
🏆 Productivity Consistency: Maintaining consistent productivity levels rather than cycling between paralysis and hyperactivity.
Timeframe Expectations:
⏱️ First 2 Weeks: Increased awareness of ADHD-anxiety interaction patterns.
⏱️ 1-2 Months: Noticeable improvement in ability to interrupt rumination cycles.
⏱️ 3-4 Months: Significant reduction in "analysis paralysis" episodes.
⏱️ 6-12 Months: Integration of management strategies into daily life with substantial symptom improvement.
Quick Cheat Sheet (Summary of Key Takeaways)
🔹 ADHD and anxiety create a neurobiological "perfect storm" in the brain, with overlapping effects on the prefrontal cortex, amygdala, and neurotransmitter systems.
🔹 Rumination in ADHD tends to be task-related, future-oriented, and self-critical, often differing from the patterns seen in primary anxiety disorders.
🔹 "Analysis paralysis" represents the intersection of executive dysfunction and anxiety, creating a state where overthinking prevents action.
🔹 Effective treatment typically requires addressing both conditions, often combining medication approaches with targeted cognitive-behavioral strategies.
🔹 Body-based interventions like brief movement, breathwork, and mindfulness create "pattern interrupts" that can break rumination cycles.
🔹 External scaffolding through environmental modifications reduces cognitive load and helps bypass anxiety triggers.
🔹 Consistency trumps perfection – small, regular implementations of management strategies ultimately yield greater benefits than sporadic intensive efforts.
Further Reading (Books & Resources)
📖 "Taking Charge of Adult ADHD" by Russell A. Barkley – Amazon Link
📖 "The Anxiety and Worry Workbook: The Cognitive Behavioral Solution" by David A. Clark and Aaron T. Beck – Amazon Link
📖 "Mindfulness for Adult ADHD: A Clinician's Guide" by Lidia Zylowska and John T. Mitchell – Amazon Link
📖 "Focused Forward: Navigating the Storms of Adult ADHD" by James M. Ochoa – Amazon Link
📖 "Cognitive-Behavioral Therapy for Adult ADHD" by Mary V. Solanto – Amazon Link
Practical Tools & Apps
🔧 Headspace's ADHD Meditation Collection – Website Link
🔧 Todoist for flexible task management – Website Link
🔧 Brain.fm for focus-enhancing music – Website Link
🔧 Delay Timer app for implementation intentions – Website Link
🔧 Freedom app for blocking distractions – Website Link
🔧 Calm Harm app for managing emotional intensity – Website Link
Research & Studies Section (Citations & Sources)
Kessler, R. C., et al. (2006). The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry, 163(4), 716-723.
Shaw, P., et al. (2007). Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences, 104(49), 19649-19654.
Posner, J., et al. (2014). Abnormal amygdalar activation and connectivity in adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 53(3), 283-292.
Edel, M. A., et al. (2013). Differential effects of methylphenidate and atomoxetine on attentional processes in children with ADHD: An event-related potential study using the Attention Network Test. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 40, 130-138.
Mohan, A., et al. (2016). The significance of the default mode network (DMN) in neurological and neuropsychiatric disorders: A review. The Yale Journal of Biology and Medicine, 89(1), 49-57.
Geffen, J., & Forster, K. (2018). Treatment of adult ADHD: A clinical perspective. Therapeutic Advances in Psychopharmacology, 8(1), 25-32.
Anastopoulos, A. D., et al. (2018). Cognitive-behavioral therapy for college students with ADHD: Temporal stability of improvements in functioning following active treatment. Journal of Attention Disorders, 22(14), 1317-1327.
Zylowska, L., et al. (2008). Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. Journal of Attention Disorders, 11(6), 737-746.
Cortese, S., et al. (2016). Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. The Lancet Psychiatry, 5(9), 727-738.
Mitchell, J. T., et al. (2017). A pilot trial of mindfulness meditation training for ADHD in adulthood: Impact on core symptoms, executive functioning, and emotion dysregulation. Journal of Attention Disorders, 21(13), 1105-1120.
What Now?
Breaking free from the cycle of ADHD and anxiety isn't about perfection—it's about progress. Start by implementing just one strategy from this article this week. Notice the patterns of rumination without judgment, and remember that understanding the neurobiological basis of these challenges removes blame and shame. With consistent practice and the right support, the intertwined challenges of ADHD and anxiety can become more manageable, allowing your natural strengths and abilities to shine through again.
🎧 For more insights, check out this ADHD podcast:























Share this post